Posted on: 13/August/2025 | By Dr. Ritesh Gaikwad
Gangrene: How Modern Vascular Surgery Can Save Your Limb
Introduction
“Blackened toe,” foul smell, or a wound that simply won’t heal can be frightening—but gangrene is often salvageable if treated early. At my centers in Thane (Ghodbunder Road, KIMS Hospital) and Mumbai (Ghatkopar, Mulund), we use modern endovascular techniques and advanced wound care to control infection, restore blood flow, and save limbs.
What is Gangrene?
Gangrene is tissue death due to poor blood supply and/or infection.
Types:
- Dry gangrene: from critical ischemia (very poor blood flow), often in toes/feet.
- Wet gangrene: ischemia plus infection; progresses quickly and needs urgent care.
- Gas gangrene: aggressive, toxin-producing infection—medical emergency.
Who is at Risk?
- Diabetes, Peripheral Arterial Disease (PAD)
- Smoking, high cholesterol, uncontrolled hypertension
- Chronic kidney disease, dialysis patients
- Foot trauma, ill-fitting footwear, previous ulcers or surgeries
Early Warning Signs You Shouldn’t Ignore
- Persistent pain or numbness; leg pain on walking or at rest
- Color change: pale → blue → black; coldness of toes/foot
- Foul smell, pus, or rapidly worsening wound
- Fever or feeling unwell (suggests infection spreading)
Act within hours—not days—if infection is suspected. Early action is the difference between a minor procedure and an amputation.
How We Diagnose the Cause (Quickly)
- Bedside vascular exam and wound assessment
- Doppler/ABI and Duplex ultrasound to map blood flow
- CT/MR Angiography when needed for detailed planning
- Blood tests and cultures (without delaying limb-saving treatment)
- TcPO₂/PVR for healing potential and surveillance (when appropriate)
Modern Limb-Salvage: Infection-First Protocol
Control Infection Immediately (first few hours)
- Start IV antibiotics promptly (then tailor to cultures).
- Sepsis bundle when indicated: fluids, labs, glycemic control, analgesia.
- Early involvement of ID/critical care if systemic illness.
Urgent Source Control (Debridement/Drainage)
- Remove necrotic tissue, drain pus, and decompress compartments if needed.
- Staged debridements are planned; wounds are left open initially.
- Consider limited amputation only when necessary to stop spread.
Restore Blood Flow (Revascularization After Stabilization)
- Once infection is being controlled, revascularize to enable healing:
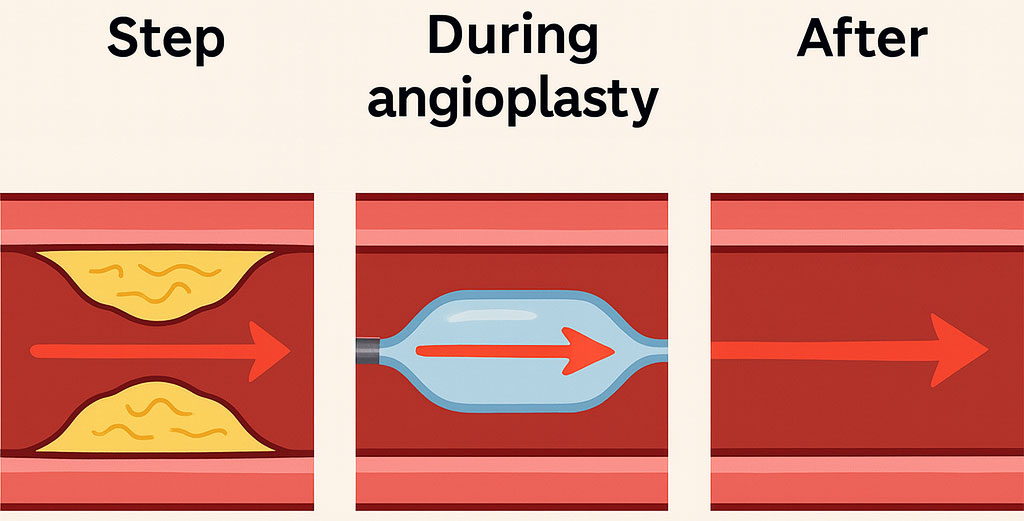
- Endovascular angioplasty & stenting as first line.
- Atherectomy for hard plaque; IVL for heavy calcium.
- IVUS-guided sizing/optimization.
- In limb-threatening ischemia, revascularization may be done early after antibiotics are started, but infection control remains the lead step.
Advanced Wound Healing
- NPWT (vacuum therapy), appropriate dressings, off-loading/footwear.
- Adjuncts when indicated: biologic dressings/skin substitutes.
Medical Optimization
- Tight sugar control, antiplatelet + statin, smoking cessation, nutrition.
Real-World Example (Name changed)
Mr. S., 87 years, presented with toe-tip gangrene and severe rest pain. He received urgent antibiotics and limited debridement first, followed by angiography, atherectomy and angioplasty. Infection settled; a limited toe amputation healed well; the leg was saved.
When is Amputation Necessary?
If infection threatens life or tissue is non-viable despite revascularization, a limited, well-planned amputation can be life-saving. Our goal is always the lowest level possible with rapid rehabilitation.
Recovery & Follow-Up
- Most patients walk early; dressings continue as per wound progress
- Surveillance plan: ABI/PVR/TcPO₂ and clinical review at 1, 3, 6, 9, 12 months, then yearly
- Long-term prevention: smoking cessation, footwear checks, foot hygiene, and strict diabetes control
Preventing Gangrene: Your Checklist
• Daily foot checks (color, cracks, callus, nails) • Control sugars, BP, cholesterol • Proper shoes/socks; avoid barefoot walking • Report any wound, discoloration, or new pain immediately • Keep follow-ups—don’t skip surveillance after treatment